January 20, 2025
By: Brionna Benedetti, CPC, CRC
Download the full guide: Cardiovascular Disease Coding Guide
Statistical Significance
According to the Cleveland Clinic, cardiovascular diseases (CVD) are defined as conditions that affect the heart and blood vessels. Conditions falling into this category of disease can also affect other organs and body systems and can lead to additional comorbidities, due to organ damage caused by decreased or blocked blood flow (1). Almost half of adults in the U.S. have some form of cardiovascular disease. Cardiovascular diseases such as coronary artery disease, cerebrovascular disease, and peripheral arterial disease are some of the leading causes of illness and death in the US. With such a large prevalence of these conditions within the United States’ population, the financial and health implications of these diseases take a steep toll:
- Cardiovascular disease (CVD) accounted for 874,613 deaths in the United States in 2019.
- Lower extremity peripheral artery disease (PAD) affects >230 million people worldwide.
- Someone in the US has a stroke every 40 seconds and dies every 37 seconds.
In the USA, the cost of cardiovascular diseases in the healthcare industry in 2015 was calculated to be over $500 billion, and this figure is climbing every year. By 2035, it is estimated that the total cost implications of these diseases will cost the nation over $1 trillion (2).
Common Cardiovascular Diseases
There are many types of diseases that fall into the CVD category, including diseases such as myocardial infarction, coronary artery disease, heart arrhythmia, valvular diseases, heart failure, peripheral vascular disease (PVD), cerebrovascular disease, aortic diseases, and deep vein thrombosis (DVT). However, in this guide we will cover the most common conditions that have a large impact on Federally Qualified Health Center (FQHC) Medicare stars and eCQM performance.
Coronary Artery Disease (CAD)
Coronary artery disease (CAD) is when major blood vessels that supply the heart struggle to send enough blood, oxygen and nutrients to the heart muscle due to plaque buildup (cholesterol deposits in an artery). CAD is the most common type of heart disease in the United States, with risk factors linked to obesity, physical inactivity, unhealthy eating habits and smoking (5). Some people experience angina (chest pain) as a result of plaque buildup, but some individuals may not experience any noticeable symptoms until the plaque triggers a blood clot or heart attack- this is why CAD is known as the “silent killer” (5).
CAD Coding Tips
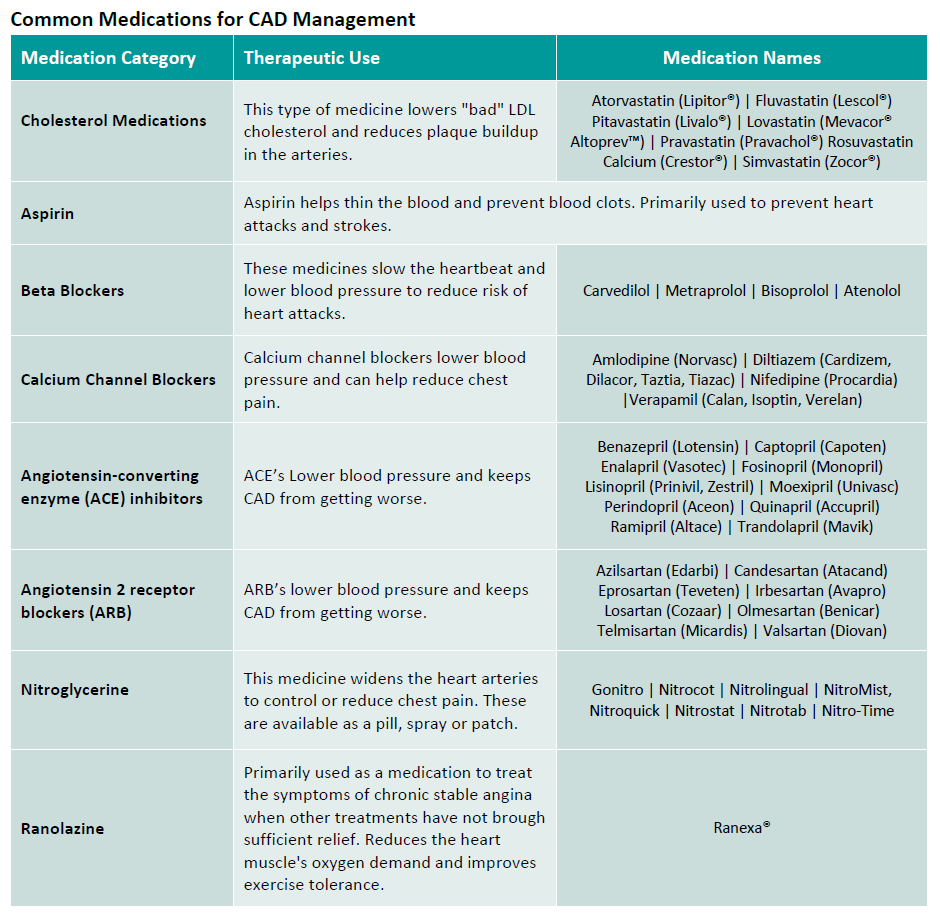
There are 40+ codes for atherosclerosis of the coronary artery alone. However, only a select grouping of CAD conditions have an HCC category in the V28 model, meaning they do not have any additional RAF (risk adjustment factor) weight to the patient’s overall RAF score. Most codes that are unspecified or do not have unstable angina will not risk adjust. Specificity is more important than ever before! To make the proper code selection you need documentation on:
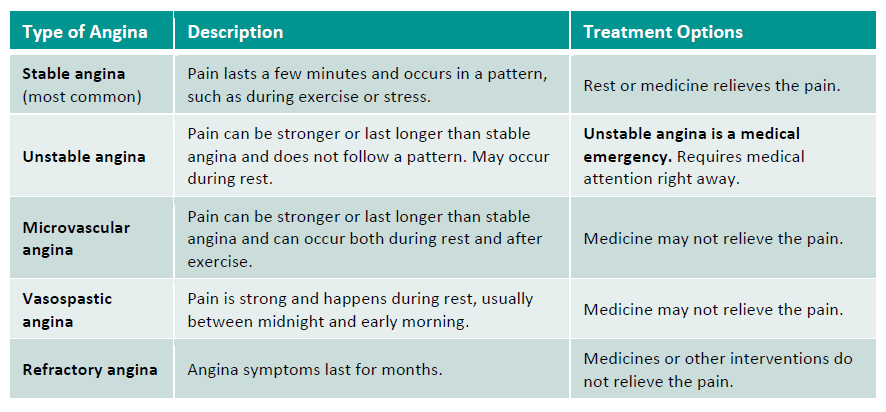
Most CAD codes no longer risk adjust in the V28 HCC model approved by CMS. The only codes that do risk adjust for CAD are for patients experiencing unstable angina pectoris. This is why it is so important to clearly specify the type of angina the patient is experiencing, if any. Do not describe current angina, or angina that is receiving treatment as “history of”, as that means the angina no longer exists.
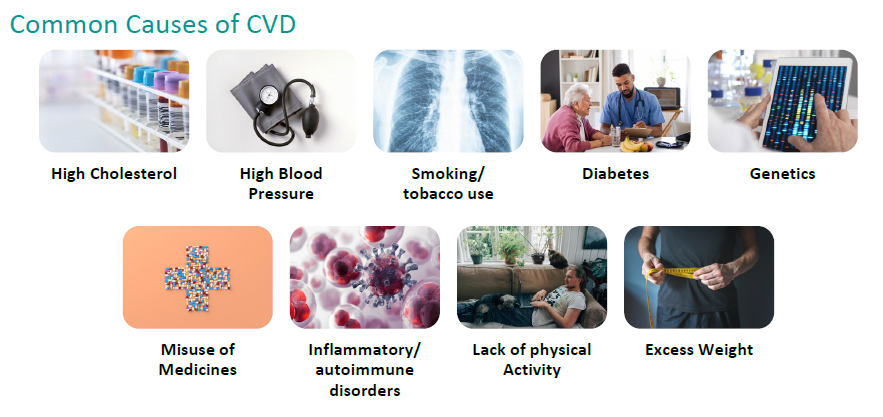
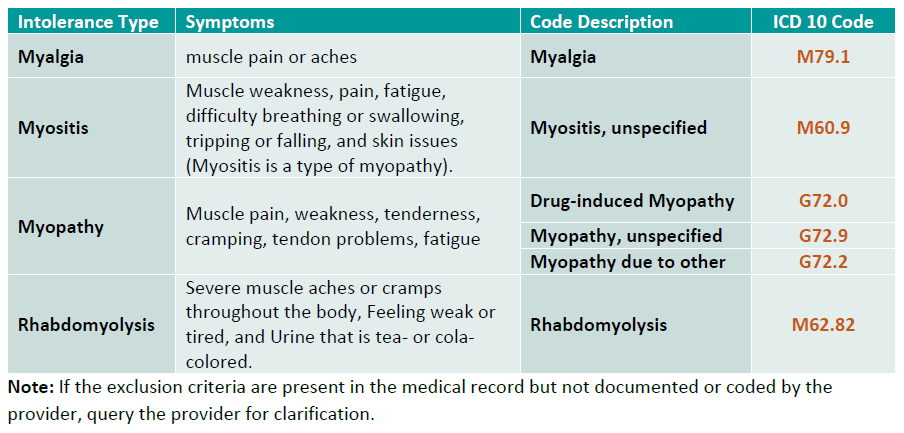
Medication Adherence Exclusions
Some patients that have CAD may experience intolerances to certain statin medications after performing a trial. These intolerances are defined as disagreeable symptoms or laboratory findings that are related to the statin treatment. If a patient experiences any of the following intolerances after taking statins, making them ineligible for statin treatment, the following exclusion criteria should be thoroughly documented in the medical record and coded. Coding for these exclusions will remove the patient from the statin medication adherence measures, commonly measured and maintained by Medicare and Medicare Advantage plans.
Heart Failure
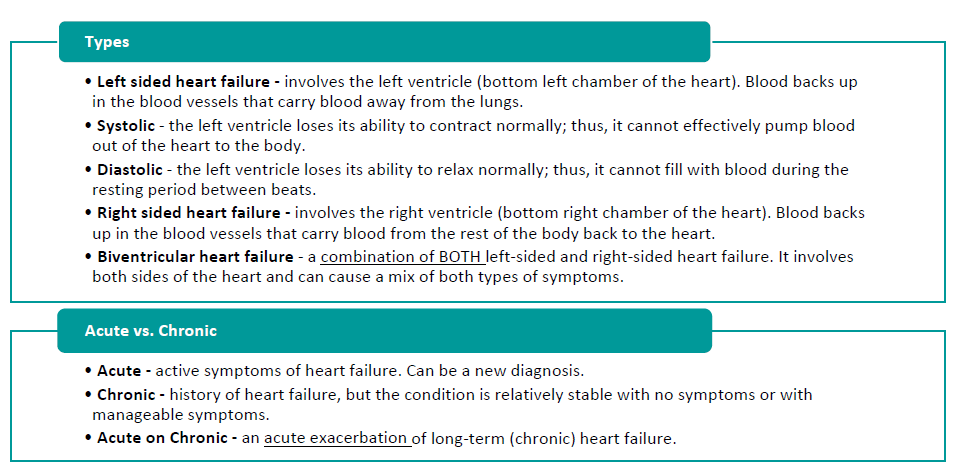
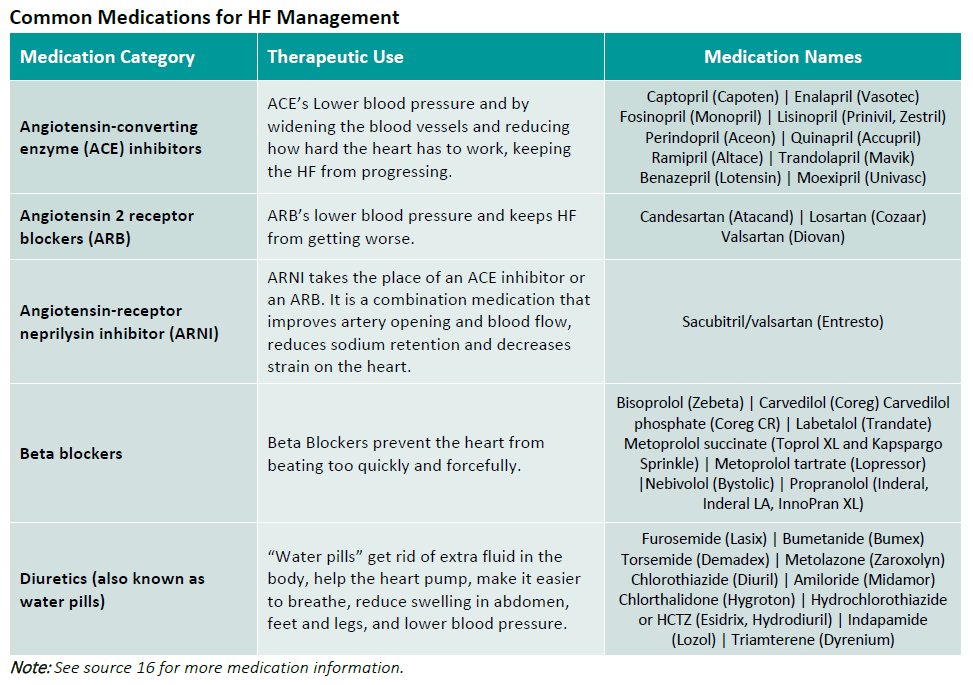
Heart failure is a condition that occurs when the heart can’t pump as well as it should, causing blood, oxygen and nutrients to struggle reaching the rest of the body. This can happen when the heart muscle becomes weak or stiff (9). People can and do live with heart failure chronically, but it can become life threatening acute condition.
To select the correct heart failure code for a patient, documentation needs to detail the type of heart failure, the cause of heart failure, if known (using linking terms to show cause and effect- “associated with,” “due to,” “secondary to,” “hypertensive,” etc.), and the current status of heart failure (stable, worsening, improved, in remission, compensated, decompensated, etc.) Even if the patient is being seen for other conditions when originally making the appointment, if the heart failure affects that patients care, management, or treatment at the time of service the heart failure should be documented and coded. Do not document “history of” to describe current heart failure. In diagnosis coding, the descriptor “history of” implies the condition occurred in the past and no longer exists. Instead, list the heart failure as stable, if being monitored and maintained.
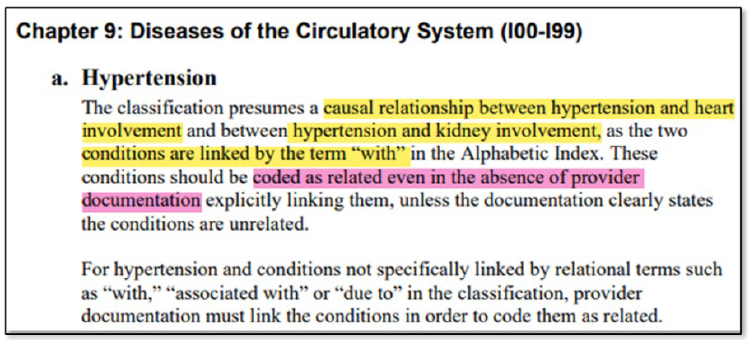
Hypertension and Heart Failure
Hypertension coding has an assumed causal correlation with chronic kidney disease (CKD) and congestive heart failure (CHF), as they are common comorbidities that exacerbate each other. This is an important distinction, as coders have the discretion to code to higher specificity even when not directly correlated in providers’ documentation. In most instances of coding, the coders are not permitted to select a more specified code on the providers behalf, but hypertension codes are unique in this way. This is extremely important, as the highly specified codes outlining these comorbidities help our stars ratings and eCQM scores for blood pressure control.
Controlling Blood Pressure Gap Exclusions
The codes for hypertension with heart disease and hypertension with chronic kidney disease are considered “advanced Illnesses” due to the complexity and severity of the diseases.
Example: If a patient is coded to have I13.0 Hypertensive heart and chronic kidney disease with heart failure and stage 1 through stage 4 chronic kidney disease, I50.32 for Congestive Heart Failure and N18.2 for CKD stage 2, this patient would effectively be removed from the controlling blood pressure denominator for most Medicare Advantage plans.
For Medicare ECQM’s, if a code for I13.0 is coded, and a frailty exclusion code (see our Advanced Illness and Frailty guide on our website for a list of frailty codes), then the patient can be excluded from the controlling blood pressure ECQM measure.
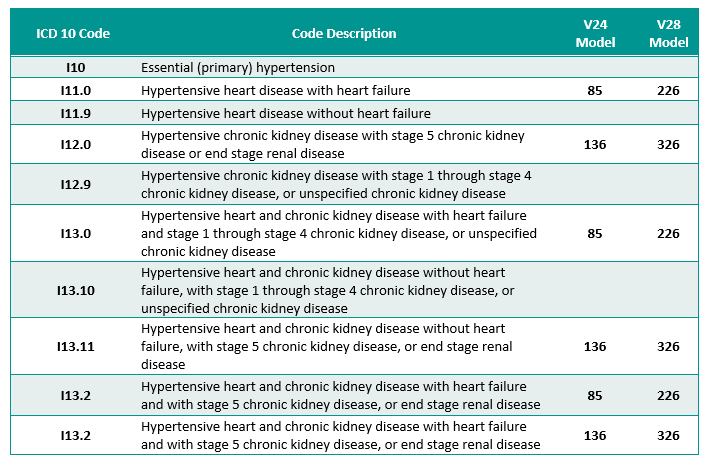
Coding I10 Essential Hypertension for a patient that has a comorbidity not only is incorrect coding, but it also negatively impacts your stars rating and eCQM scores, as it is harder to control the blood pressure of a patient with these comorbidities. Once you code I10 for the patient, they fall into the CBP denominator and will count against you if you cannot keep their BP below 140/90, especially for the last reading of the year which the payers collect to measure compliance. Specificity in documentation and code selection is advantageous for financial success and coding compliance.
Find more coding guides at https://chpanetwork.com/guides-tools/.
Sources
- Cardiovascular Disease: Types, Causes & Symptoms – Cleveland Clinic
- Economic Impacts of Cardiovascular Diseases: An Econometric Evaluation in Turkey
- Epidemiology of Peripheral Artery Disease and Polyvascular Disease
- Peripheral artery disease (PAD) – Symptoms and causes – Mayo Clinic
- Coronary Artery Disease (CAD): Symptoms & Treatment – Cleveland Clinic
- Coronary Artery Disease – Mayo Clinic
- Angina (Chest Pain) – Types
- Heart Attack: Symptoms, Causes & Treatment – Cleveland Clinic
- Heart Failure – Johns Hopkins Medicine
- Cholesterol Medications – American Heart Association
- Beta blockers for cardiovascular conditions: one size does not fit all.
- Calcium Channel Blockers
- Types of Heart Medications – American Heart Association
- Nitroglycerin (oral route, sublingual route)
- Ranolazine Extended-Release Tablets – Cleveland Clinic
- Medications Used to Treat Heart Failure – American Heart Association