About Us
About Us

Powering Value-Based Care and Community Health
CCMCN-CHPA strengthens Colorado’s community health network through value-based care innovation, data-driven solutions, and collaborative clinical support — helping our members deliver better care, improve outcomes, and thrive in a changing healthcare landscape.
-
Mission: To improve the quality and cost of care for the people our members serve.
-
Vision: To be an admired nonprofit leader in value-based care focused on individuals and communities.
-
Values
• Accountability – we rely on one another to deliver excellence and are mindful of our impact on patient care
• Adaptability – we innovate, informed by data and network needs
• Community – we build a diverse environment that is equitable and inclusive
• Compassion – we act with empathy, kindness, and understanding
Who We Are
CCMCN-CHPA is a statewide integrated network of community health organizations dedicated to advancing value-based care and improving population health. Born from the combined expertise of two long-standing leaders — Colorado Community Managed Care Network (CCMCN) and Colorado Health Providers Alliance (CHPA) — we operate as a single, unified organization to better support our members and the communities they serve.
Our Mission
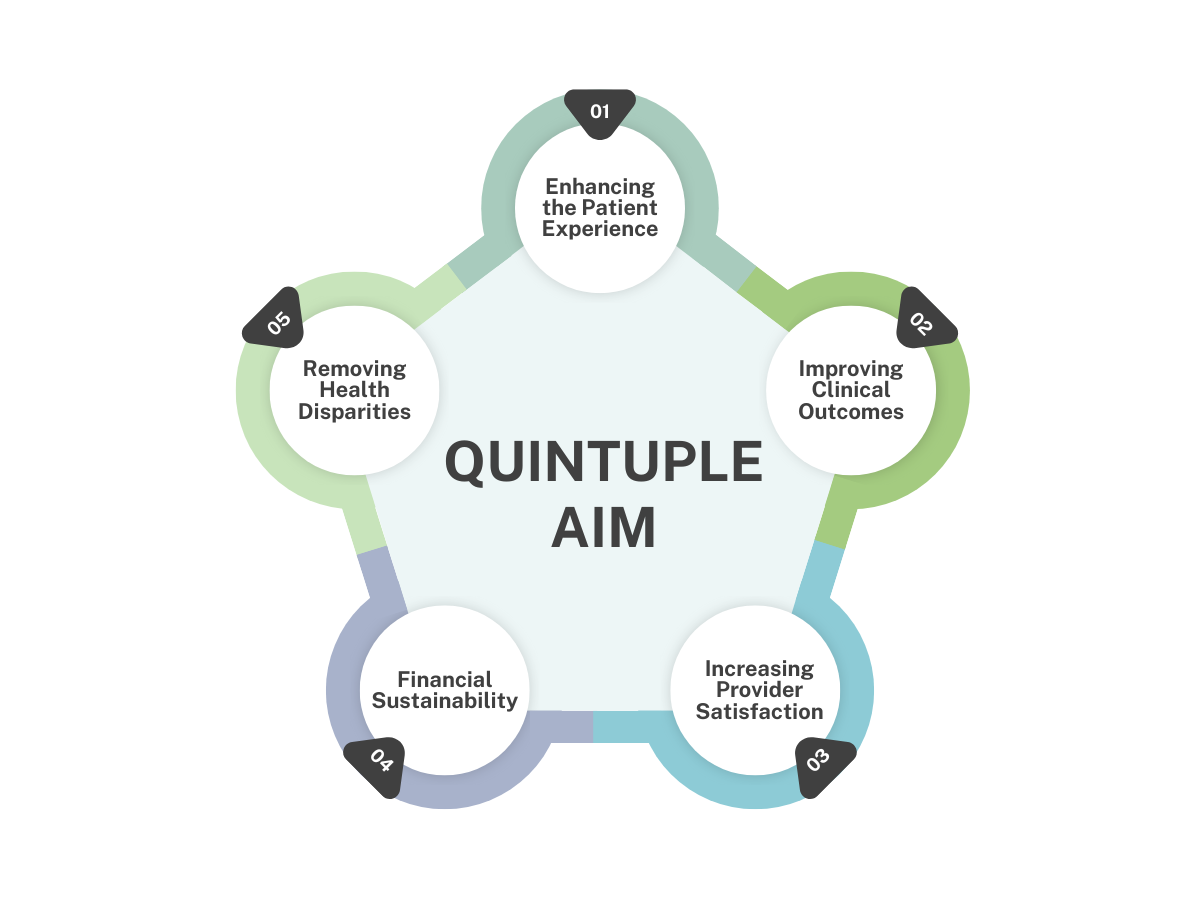
We help our member organizations succeed under value-based models by improving quality outcomes, enhancing patient care, supporting provider well-being, and delivering smarter, more sustainable healthcare. Our work is guided by the goals of the Quintuple Aim.
What We Do
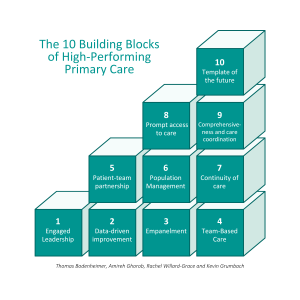 We deliver the strategies, tools, and partnerships community health centers need to excel, including:
We deliver the strategies, tools, and partnerships community health centers need to excel, including:
- Value-Based Care Support: Helping members meet quality, cost, and patient-centered care goals through clinical integration, medical coding education, and practice transformation coaching.
- Data and Analytics: Turning population health data into actionable insights that drive smarter decision-making and targeted interventions.
- Care Coordination: Building stronger links across providers, payers, and community resources to support whole-person care.
- Member Collaboration: Fostering a trusted network where members align, innovate, and succeed together.
Our Impact
By combining clinical expertise, powerful data systems, and a culture of collaboration, CCMCN-CHPA empowers health centers to deliver better outcomes and create lasting change in the communities they serve.
Subscribe To Our Newsletter