By: Brionna Benedetti CPC, CRC
Download the printable version
An Ode to Neoplasms
“Ere frost-flower and snow-blossom faded and fell, and the splendour of winter had passed out of sight… March, master of winds, bright minstrel and marshal of storms that enkindle the season they smite” [2].
March has played a pivotal role in inspiring many influential periods and pieces in history, including Algernon Charles Swinburne, the author of “March: an Ode”. March also brings revived importance to understanding the future of preventative care, especially as it pertains to colorectal cancer awareness month.
Colorectal cancer is the third most diagnosed cancer in the United States, with the American Cancer Society estimating that in 2024, the United States will have approximately 106,590 new cases of colon cancer and approximately 46,220 new cases of rectal cancer; affecting more men than women on average [1]. The mortality rate from colorectal cancer for individuals over 55 has been falling in recent years and is associated with more abundant usage of preventative screenings leading to: 1) finding and removing polyps before they can further develop, and 2) detecting colorectal cancers earlier when they are easier to treat. For individuals under 55, however, death rates have been increasing by about 1% annually since the mid-2000s [1]. With these statistics in mind, we take a moment to educate our network and community on how we as medical professionals can do our part to ensure that these cancers are properly addressed and reported within our everyday practice.
Neoplasm Coding and Documentation
In the ICD-10-CM cancer codes are held in the code range C00-D49, with some exceptions to cancers that are commonly found within a specific body system. To select the proper cancer code, the medical record should be as accurate and detailed as possible with notation of the site and laterality, stage, and behavior of the cancer if known, and if the cancer is currently being treated or if the treatment has resolved and is considered past medical history. Coders utilize this detailed information to select the proper code by searching through the “Table of Neoplasms” within the ICD-10-CM, and confirming the code selection in the tabular list.
Site and Laterality
Neoplasm codes heavily rely on the documentation of the location and whether it is primary or secondary in nature, and (depending on the limb) if the malignancy is unilateral or bilateral for proper code selection. A primary malignancy is where the cancer originates inside the body, and a patient can have multiple primary sites for cancer in the body at the same time. A secondary malignancy is when the cancer has spread to that organ or site from the original primary location of the cancer (document “metastatic, “or “secondary”) [4]. Here is an example of how important this distinction is in code selection: when coding for a malignant cancer of unspecified behavior found on the upper right arm, a sixth character is needed to identify the right-sided laterality.
- The correct code: C44.602 Unspecified malignant neoplasm of skin of right upper limb, including shoulder.
- If laterality was not identified, the code selection would default to: C44.601 Unspecified malignant neoplasm of skin of unspecified upper limb, including shoulder.
- If a neoplasm is malignant and has spread to a secondary location, the site of the original neoplasm and the secondary neoplasm should both be clearly documented to ensure the correct codes are selected.
Stage
To properly code for a malignant neoplasm, the medical record should clearly state if the neoplasm is benign, in-situ (abnormal cells that have not spread from the location where they first formed [3]), malignant or of uncertain behavior when known. The term “neoplasm of uncertain behavior” is a specific pathologic diagnosis. This is a lesion whose behavior cannot be predicted. Uncertain behavior can mean the mass is currently benign, but there’s a chance that it could undergo malignant transformation over time. ICD-10-CM manual indicates that these are “certain history-morphologically well-defined neoplasms, the subsequent behavior of which cannot be predicted from the present appearance” [4]. If the documentation is unclear about the stage of the cancer, it is advised that the coder query the provider for clarification before a code is selected.
Active vs. Past Medical History
One of the most complex parts of coding for cancers as a primary care physician can be determining whether a cancer is active versus past medical history, especially if documentation from outside specialists and oncologists is unclear. However, the treatment plan of a cancer diagnosis is a key element needing documentation in the medical record when it comes to coding for cancers. If a primary cancer has been excised but still requires continued treatment (i.e. additional surgeries, radiation therapy, chemotherapy) to obtain remission at the specific site, the primary malignancy code should be coded until the treatment is completed [4].
Once all treatment to the site has ceased and there is no further evidence of the malignancy to the site, a code from Z85.0-Z85.5 should be assigned to show the past medical history of the malignancy depending on the location. Codes within this range should only be assigned for a primary malignancy, not for the site of a secondary malignancy. Code Z85.89 can be assigned for both primary and secondary malignancies of historical origin [4].
Quality Measure Screenings and Exclusion Codes
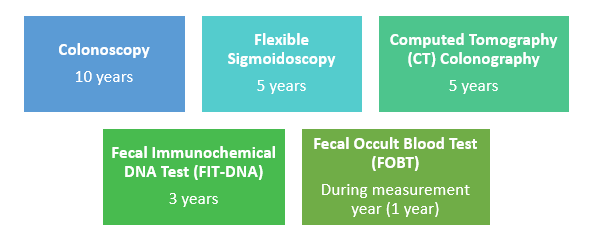
Regular preventative screening for colorectal cancer should begin at age 45 and should be continued until the patient is 75 years of age. To close the care gap for the patient, documentation of a viable colon screening within the medical record must include a note indicating the type of screening done, the date (MM/YYYY) on which the screening was performed, and the results of the findings (normal, abnormal, positive, negative). The frequency of screening is dependent on the type of screenings used and how long each screening type is viable for per CMS:
Measure Exclusions
Members 66 years of age and older as of December 31 of the measurement year who meet either of the following:
- Total Colectomy documented within the medical record (partial colectomy does not count).
- Colorectal Cancer.
- Patients who had a claim of hospice/palliative care, or documentation of hospice/palliative care.
- Patient was enrolled in an Institutional SNP any time in the measure year.
- Patients with two advanced illness codes and two advanced frailty codes billed at two separate outpatient or non-acute inpatient visits within the calendar year.
Acceptable Advanced Illness Codes:
| Code | Code Description |
| C78.4 | Secondary malignant neoplasm of small intestine |
| C78.5 | Secondary malignant neoplasm of large intestine and rectum |
| C78.6 | Secondary malignant neoplasm of retroperitoneum and peritoneum |
| C78.7 | Secondary malignant neoplasm of liver and intrahepatic bile duct |
| C78.80 | Secondary malignant neoplasm of unspecified digestive organ |
| C78.89 | Secondary malignant neoplasm of other digestive organs |
Sources:
1. Colorectal Cancer Statistics | How Common Is Colorectal Cancer? | American Cancer Society
2. March: An Ode by Algernon Charles Swinburne | Poetry Foundation
3. Carcinoma in Situ: Stage 0 Cancer That Hasn’t Spread (cancercenter.com)
4. ICD-10-CM