By: Brionna Benedetti, CPC, CRC
Download the full guide: Queries: The 5 W’s of Effective Communications
What is a Query?
The American Health Information Management Association (AHIMA) defines a query as a “communication tool or process used to clarify documentation in the health record for documentation integrity and accuracy of a diagnosis/procedure/service code(s) assignment for an individual encounter in a healthcare setting” (2).
Why are Queries Important?
Billing and coding professionals use queries to support the assignment of correct code(s) based on clinical documentation. Queries are the key to increasing the precision of clinical documentation, which in turn promotes accurate clinical data, accurate depiction of patient acuity, and appropriate code selection for the encounter codes and diagnoses (1).
When to Send a Query
Billing and coding professionals send queries when they identify that the health record does not meet one of the following criteria: legibility, completeness, clarity, consistency, precision, reliability, or timeliness. Electronic medical record (EMR) systems have reduced some barriers to the legibility and reliability of a medical record, therefore, we will focus on the completeness, clarity, consistency, and precision of the medical documentation.
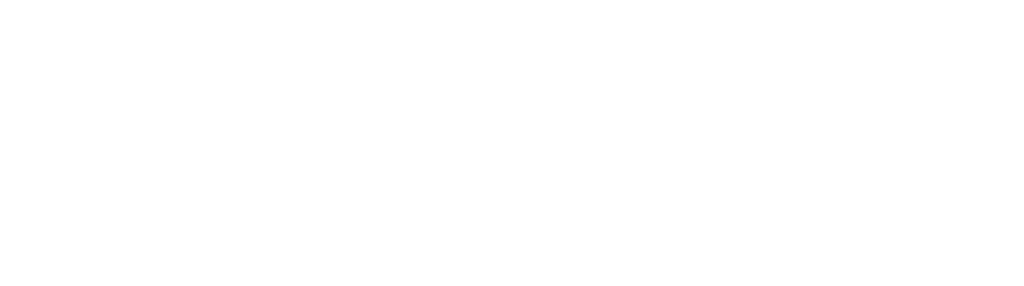
Specificity
Specificity in documentation is vital to appropriate code selection and can be one of the more challenging barriers coders face. Billers and coders are not permitted to make what could be considered reasonable assumptions based on the medical record and rely on the provider’s complete and accurate documentation to effectively select a code(s). Specificity of a documented diagnosis avoids reporting a default or unspecified code that does not capture the true acuity of the patient’s care and may not risk adjust (1).
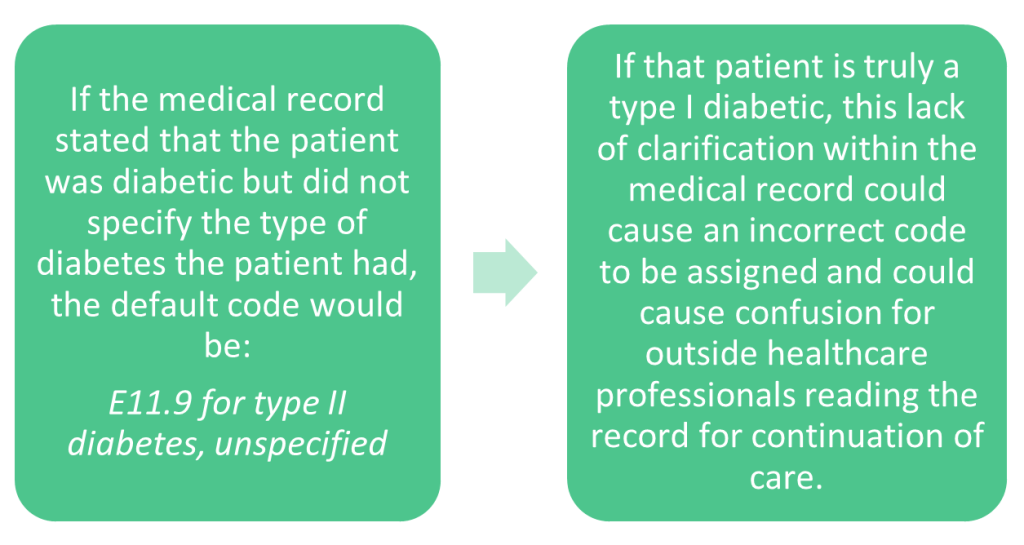
Cause and Effect Relationships
Establishing a diagnostic cause-and-effect relationship between medical conditions has a direct effect on code selection (1). Connecting comorbidities and complications in the medical record using linking terms like “and,” “with,” “due to,” and “caused by” can vastly alter code selection, the risk adjustment factor (RAF) score of a patient, and ultimately provide appropriate reimbursement to care for that patient’s level of acuity.
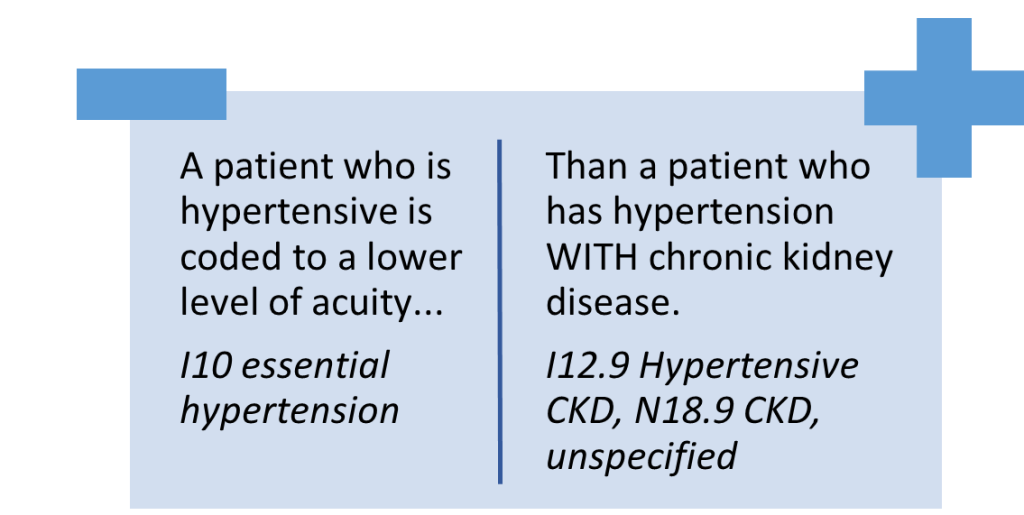
Acute vs. Chronic
Clarification of a patient’s severity can be necessary when it appears that a documented diagnosis is not clinically supported with appropriate documentation. How the patient’s condition manifests can directly alter code selection and must be clarified before a claim can be submitted.
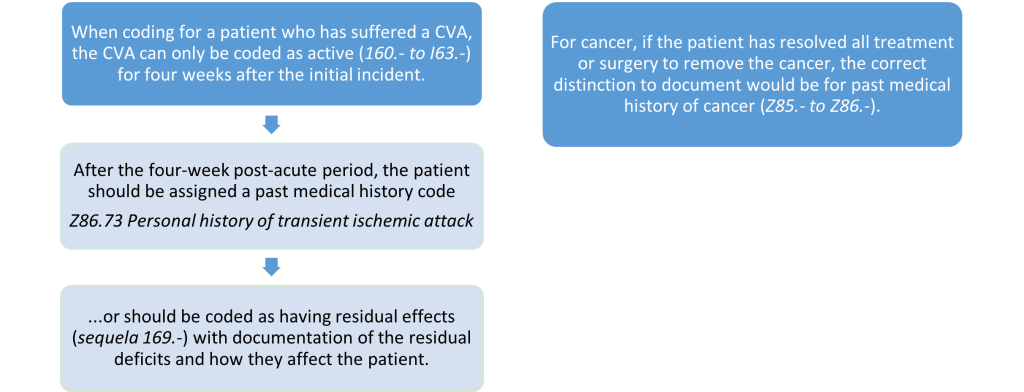
Active vs. Past Medical History
Queries are necessary when establishing the relevance of a condition documented as a “history of” to determine if the condition is active and not resolved (1). This is especially important for extreme cases like cerebrovascular accidents (CVA), or cancer.
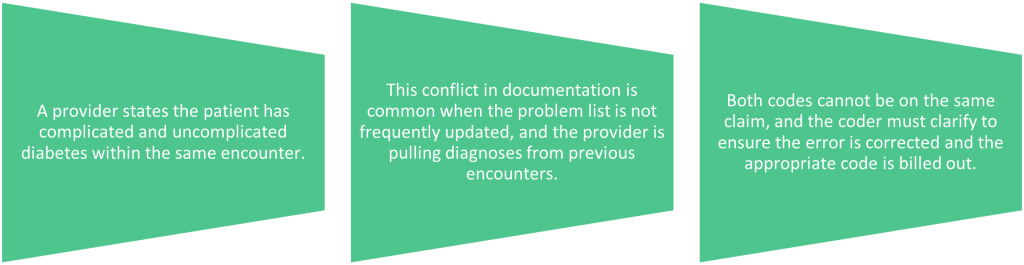
Conflicting Code Assignment
When the assessment and plan do not line up with the diagnoses selected, it can cause a conflict in the medical record. The problems lists and treatment plans should be regularly updated to avoid discrepancies. An example of how this can happen:
Where to Send a Query
Queries can be given in many forms including verbal, written, and electronic. With the widespread use of internal EMR communications, this is the most common platform for coder-to-provider communications. Regardless of the method of query, communications must adhere to compliant, non-leading standards that allow the provider to give an unbiased response with a specific diagnosis or procedure based on their clinical judgment. Queries should be documented within the patient’s health record, either as part of the office visit note, an addendum, or saved in another area that is linked to the date of service in question (1).
How to Send an Effective Query
When sending a query to a provider, consider the following options for writing your query, based on the need:
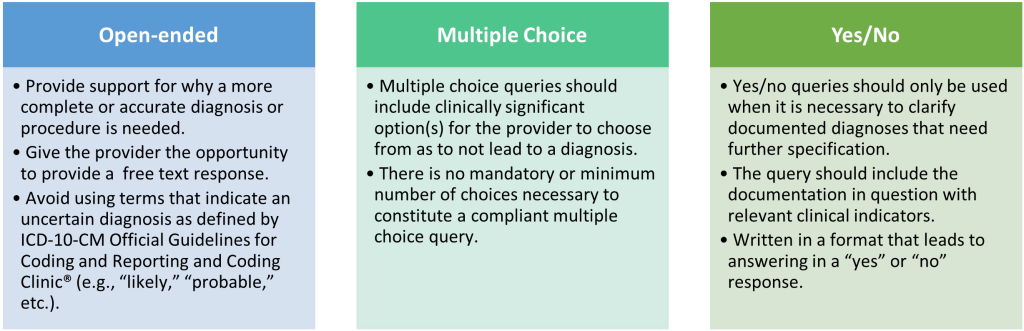
Provider responses to a query should be documented in the health record. Do not indicate the impact on reimbursement, payment, or quality metrics within your message, as this information can be considered leading and may come across as pushing a provider to a particular diagnosis or outcome. While organizations are free to determine their query process, compliant query practices require that all queries either be a permanent part of the record or be retrievable in the business record (1). Remember that what you send a provider is a part of the patient’s medical record and should be treated with care.
Writing Tips:
- Avoid inflexible statements when communicating coding concepts to providers, such as “You cannot use that Dx,” or “That is not the right way to level a 99215 visit…”
- Use factual statements such as “The Centers for Medicare and Medicaid Services (CMS) requires…”
- If there is a coding misunderstanding, be curious about their reasoning and ask questions. Give feedback with compassion when possible and be willing to educate and give resources for learning with patience.
- Use the phase, “help me understand…,” to kindly and respectfully ask for clarification.
- Bring data supporting appropriate coding guidelines to the discussion and give the provider options.
References:
1. ACDIS: Guidelines for achieving a compliant query practice (2019 Update)
2. AHIMA and ACDIS: Guidelines for Achieving a Compliant Query Practice (2022 Update)